You go to check your voicemail after a long day of seeing clients and you hear the message you’ve been dreading. It’s a representative from an insurance company wanting to do a care review on one of your clients and they’ve asked you to call them back. AHHHHH—but wait!
Don’t panic.
You’ll be just fine.
I’ve had many of these phone calls throughout the years and every time the person on the other end of the phone was pleasant/friendly and asked me basically the same questions.
Here are some tips to get you through it:
- Have the client’s chart in front of you and skim over their intake note and treatment plan prior to calling the representative back.
- This may seem obvious, but reading over the intake note will help jog your memory of the client and why they came to see you in the first place.
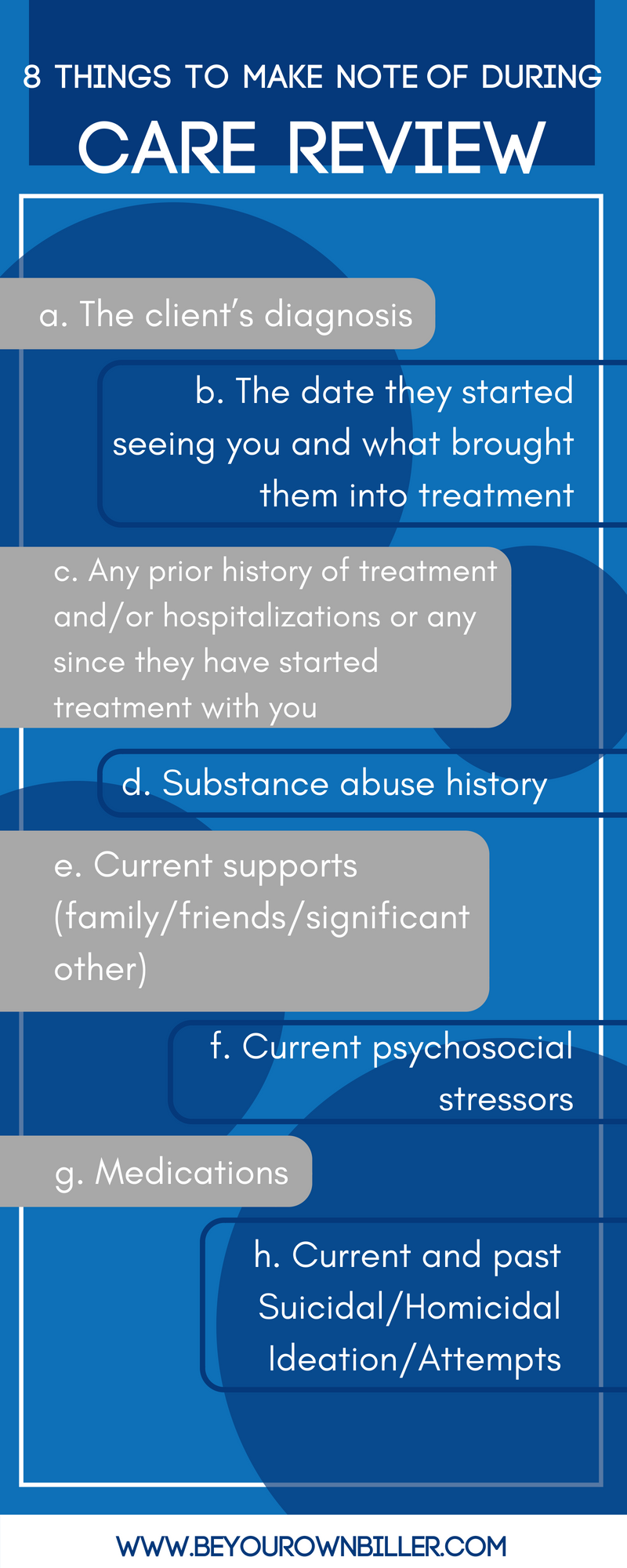
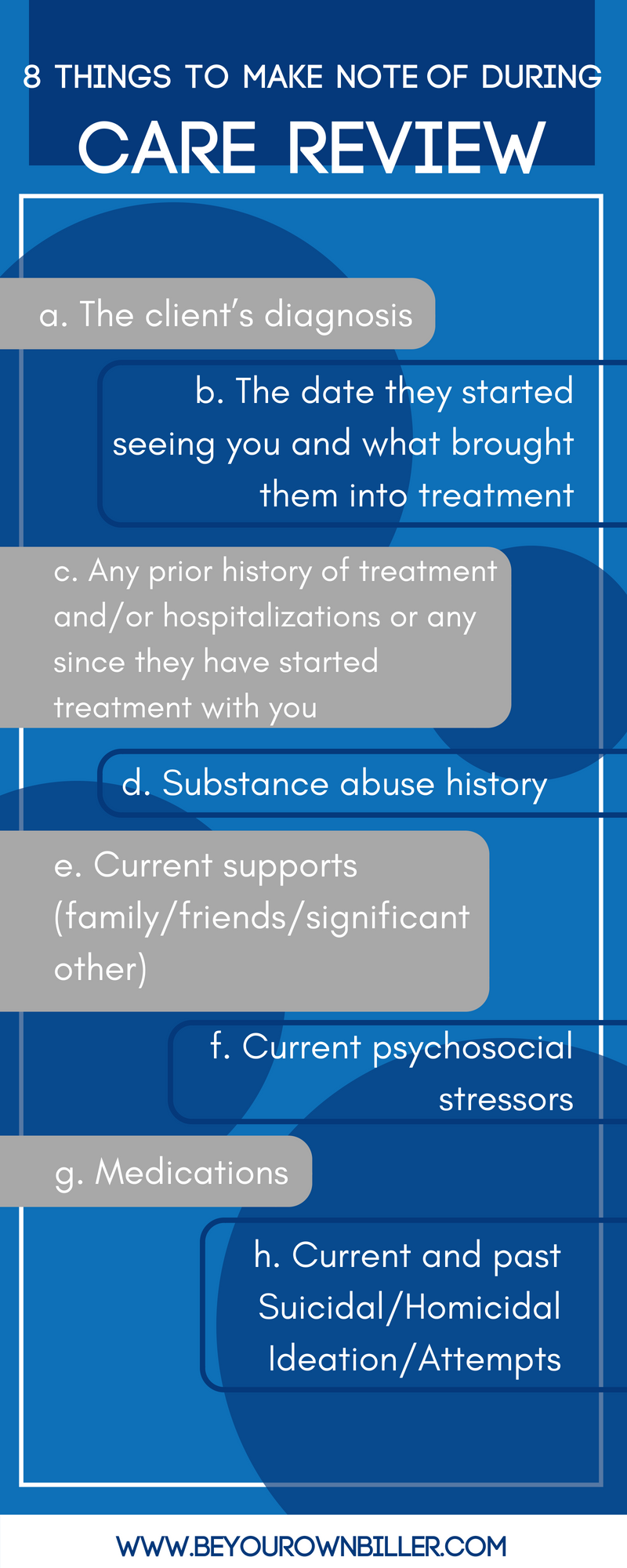
- Some things to make note of:
- The client’s diagnosis
- The date they started seeing you and what brought them into treatment
- Any prior history of treatment and/or hospitalizations or any since they have started treatment with you
- Substance abuse history
- Current supports (family/friends/significant other)
- Current psychosocial stressors
- Medications
- Current and past Suicidal/Homicidal Ideation/Attempts
- Look up their diagnosis in the DSM.
- Even if you have been using DSM terminology in your notes, the care reviewer will want to see that the client has met medical necessity for the diagnosis. I’ve found it always helpful to give the DSM dx a once over so that it is fresh in my mind before making the call.
- Be prepared to speak about their treatment goals and what approaches/interventions you have been using to reduce their symptoms.
- Evidence-based treatment interventions
- Be prepared to give an estimated length of treatment and what your plan is moving forward.
- Stick to the facts. Be concise and clear.
Remember that the care reviewer is almost always a clinician, just like you, and they are doing their job.
They are not trying to recoup money from you or catch you in some sort of act. They are checking in on the client’s progress. Often times they offer helpful tips or resources that are available to the client on the insurance company’s website.
Don’t put off calling them back—the phone call should take 15-20 minutes and if you delay calling them, it could pose problems for you with reimbursements. It will look bad—just call them back.
Once you give them some clinical on the client, they most likely won’t call you back regarding this client for another 6 months or so, but might after then to check-in on the client’s progress.
Repeat after me:
“The treatment I am doing is preventing a higher level of care. If the client were not receiving treatment from me, they may eventually have to be hospitalized.” This is the golden rule of care reviews.
I hope this helps ease some anxiety involved with care reviews!