Here are some tips to ease out of network billing confusion:
What/Who is Out Of Network?
- Clinicians who have not signed a contract with an insurance company and do not have to abide by a contracted rate.
- Can still be subject to insurance audits for medical necessity and are still considered a HIPAA-covered entity.
- Some plans may not have out of network benefits at all.
- Never guarantee a client that they will get reimbursed for seeing you out of network.
- Usually, OON has very high deductibles which means the client (or you) would not get reimbursed until the deductible is met.
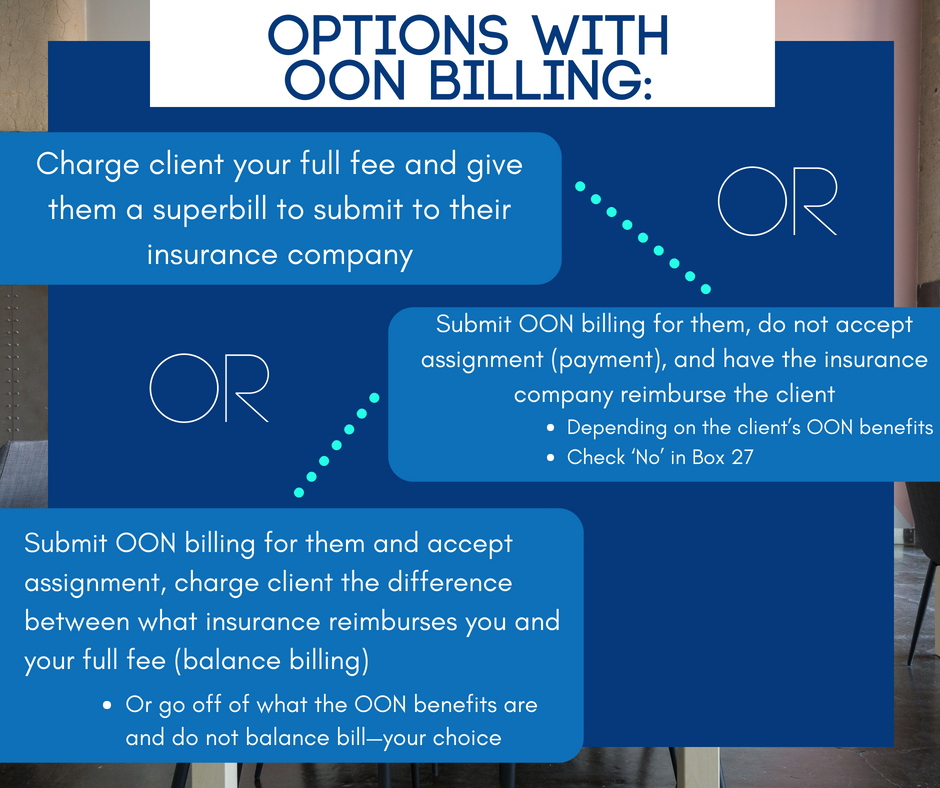
Options with OON billing:
- Charge client your full fee and give them a superbill to submit to their insurance company (Recommended!)
- Submit OON billing for them, do not accept assignment (payment), and have the insurance company reimburse the client
- Depending on the client’s OON benefits
- Check ‘No’ in Box 27
- Submit OON billing for them and accept assignment, charge client the difference between what insurance reimburses you and your full fee (balance billing)
- Or go off of what the OON benefits are and do not balance bill—your choice
Superbill
- Itemized bill given to clients to submit to their insurance company for payment
- Can only do this if you are OON
- Has the same information that is on a claim form including:
- Client’s demographic information
- Insurance information, date of birth, address
- Your EIN/NPI/License Number
- The client’s diagnosis
- CPT code and description
- What you are charging insurance and what the client paid you
- Client’s demographic information
Usual Customary and Reasonable Rate
- Think of it like an unofficial out of network rate (without a contract)
- Established to protect insurance companies from paying at the mercy of whatever providers charged
- Insurance companies take an average of each CPT code billed by providers with the same licensure level in your region to determine UCR
- This is why you should bill your full fee to insurance companies.
- Works like a contracted rate, but you can balance bill
- Example A:
- Client has an OON deductible of $2,000 and the UCR is $100
- You bill the client and the insurance company $150
- The insurance company only applies $100 towards the deductible, but you can charge the client higher than the UCR due to not being in-network.
- This is called ‘balance billing’ and is acceptable to do due to being OON and not having a contract with the insurance company. This is a contract violation if in-network as you have to collect your contracted rate and cannot balance bill.
- Example B:
- Client has met their OON deductible and insurance is paying 80% co-insurance, UCR is $100
- You bill the client and give the client a superbill with a $150 charge on it
- The insurance company reimburses the client $80 (based off of the UCR and not what you billed the client).